In the rapidly evolving landscape of healthcare, the imperative to improve patient outcomes and streamline healthcare delivery has never been more critical. However, the challenge faced by public health organizations and healthcare entities alike is the siloed nature of data and information systems. The lack of interoperability, or seamless data exchange between disparate systems, hampers the ability to provide cohesive, patient-centric care. As the digital front door to healthcare services becomes increasingly vital, overcoming the interoperability gap emerges as a pivotal challenge.
Our Advice
Critical Insight
Numerous obstacles contribute to the prevailing interoperability issues in the healthcare sector. Legacy systems, diverse data formats, and varying standards across organizations create significant barriers to the smooth flow of information. Additionally, concerns related to data security and privacy have led to a cautious approach, further hindering interoperability efforts. These challenges not only impede real-time collaboration among healthcare providers but also compromise the ability to harness the full potential of emerging technologies such as telemedicine, AI-driven diagnostics, and predictive analytics.
Impact and Result
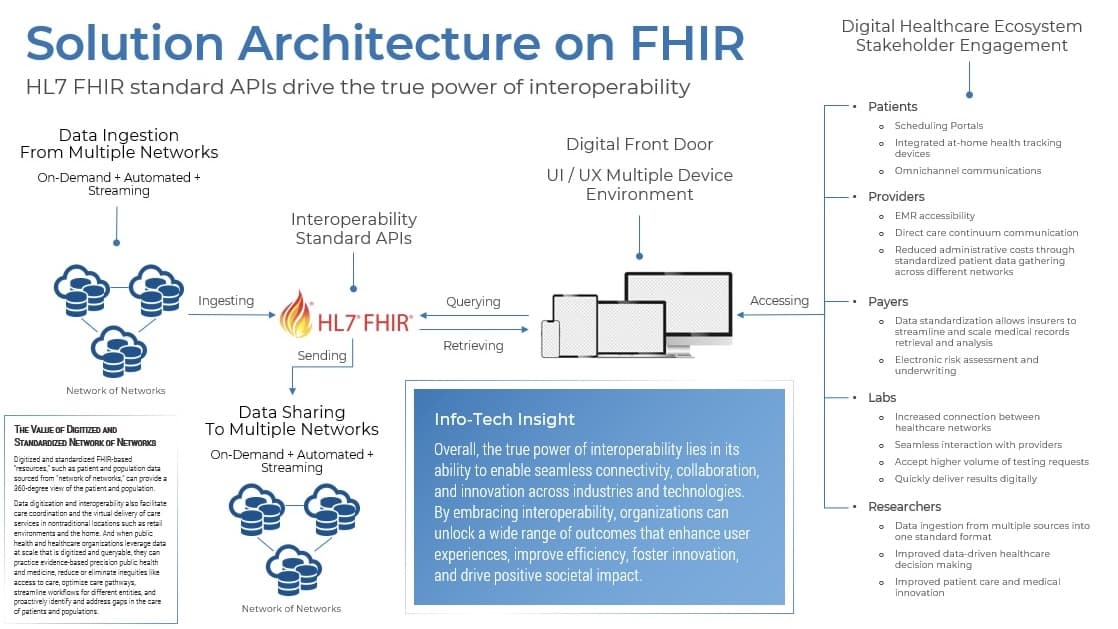
Recognizing the critical need for interoperability as the key for advancing healthcare outcomes, Info-Tech’s approach focuses on a comprehensive and adaptive strategy, including eight key insights to unlock the full potential of the digital front door. We propose the implementation of standardized data formats and protocols that enable seamless communication between disparate systems. Embracing modern technologies such as HL7 FHIR (Fast Healthcare Interoperability Resources) and SMART on FHIR, our solution facilitates the secure exchange of health information while adhering to stringent privacy standards.
Interoperability: The True Power Behind the Digital Front Door
What the Fast Healthcare Interoperability Resources mandate means for global digital health trends, and eight key insights into unlocking the full potential of the digital front door.
Analyst Perspective
At its core, interoperability breaks down the barriers that hinder effective information sharing and collaboration.
In today's rapidly evolving digital landscape, the concept of interoperability has emerged as a crucial enabler of seamless connectivity and efficient communication across various systems and platforms. It refers to the ability of different technologies, software, and devices to exchange and interpret data in a standardized and harmonious manner. While often overlooked, interoperability holds immense power behind the digital front door, revolutionizing the way we interact, collaborate, and access information. This research provides a roadmap toward overcoming the challenges and obstacles of fragmented health information, the widespread use of siloed systems, poor data quality and access, and the lack of standardization, which all lead to inefficiencies, health inequities, and AI impedance.

Neal Rosenblatt
Principal Research Director
Info-Tech Research Group
Executive Summary
Your ChallengeIn the rapidly evolving landscape of healthcare, the imperative to improve patient outcomes and streamline healthcare delivery has never been more critical. However, the challenge faced by public health organizations and healthcare entities alike is the siloed nature of data and information systems. The lack of interoperability, or seamless data exchange between disparate systems, hampers the ability to provide cohesive, patient-centric care. As the digital front door to healthcare services becomes increasingly vital, overcoming the interoperability gap emerges as a pivotal challenge. |
Common ObstaclesNumerous obstacles contribute to the prevailing interoperability issues in the healthcare sector. Legacy systems, diverse data formats, and varying standards across organizations create significant barriers to the smooth flow of information. Additionally, concerns related to data security and privacy have led to a cautious approach, further hindering interoperability efforts. These challenges not only impede real-time collaboration among healthcare providers, but also compromise the ability to harness the full potential of emerging technologies such as telemedicine, AI-driven diagnostics, and predictive analytics. |
Info-Tech’s ApproachRecognizing the critical need for interoperability as the key for advancing healthcare outcomes, Info-Tech’s approach focuses on a comprehensive and adaptive strategy, including eight key insights to unlocking the full potential of the digital front door. We propose the implementation of standardized data formats and protocols that enable seamless communication between disparate systems. Embracing modern technologies such as HL7 FHIR and SMART on FHIR, our solution facilitates the secure exchange of health information while adhering to stringent privacy standards. |
Info-Tech Insight
By leveraging interoperability as the new power behind the digital front door, and by focusing on standards-based interoperability to seamlessly drive and deliver health resources and optimize health outcomes for the individuals and populations they serve, public health organizations and healthcare entities can unlock unprecedented opportunities for coordinated care, data-driven decision-making, and improved patient experiences.
Public health and healthcare organizations prioritizing interoperability will improve data capacity and capability
This will seamlessly ensure rapid, safe, secure, and efficient gathering, sharing, analyzing, and reporting of electronic health information, resulting in reduced costs and improved health at both the individual and population level.
Providers
90% |
The percentage of providers using EMR/EHR technology. |
72% |
The percentage of providers using certified EMR/EHR technology. |
Across All Hospital Types
95% |
The percentage that have certified EHR technology. |
70% |
The percentage integrating data into their EHRs from sources outside their health systems. |
Social Determinants of Health
70% |
The percentage of providers recording SDOH patient information into their EHRs. |
What is interoperability and why is it important?
Interoperability refers to the ability of two or more computer systems to exchange, communicate, and make use of information to optimize health outcomes for individuals and populations.
To achieve interoperability, we must adopt and optimize electronic health record (EHR) technology and health information exchange (HIE) services. For health and healthcare organizations, standards-based interoperability enables authorized users from multiple locations to access, gather, integrate, and share electronic health information quickly and securely. Outcomes include better care coordination among healthcare organizations and improved nowcasting, forecasting, and scenario modeling among health and human services organizations.
We have reached the tipping point. Nearly 90% of providers use EMR/EHR technology and 72% use certified EMR/EHR technology. Nearly 70% are recording social determinants of health information. Across all hospital types, more than 95% have certified EHR technology and 70% are integrating data into their EHRs from sources outside their health systems. Like EHRs, HIE services must also be optimized, adopted, standardized, and used by healthcare providers, their patients, and public health practitioners in order to advance interoperability.
It will take time for all types of health IT to be fully interoperable. When interoperability is achieved across health and healthcare systems and the widespread exchange of information becomes standard practice, providers and health and human services organizations will have the infrastructure to deliver patient-centric and population-centered, value-driven, accountable care that improves health outcomes while reducing costs.
Source: “Interoperability,” HealthIT.gov, 2023
The digital front door has unlocked countless opportunities for efficiency, convenience, and accessibility
Value |
Objective |
Description |
| Efficiency | Cost Efficiency and Scalability | Without interoperability, organizations are often forced to invest heavily in custom integrations or maintaining legacy systems that don't communicate with newer technologies. Interoperability reduces these integration costs, making it easier to adapt and scale systems as needed. It fosters a flexible ecosystem, allowing organizations to choose the best tools and services for their specific needs without worrying about compatibility issues. |
| Convenience | Enhancing User Experience | Interoperability empowers the digital front door to provide a unified and cohesive user experience. When systems can communicate and share data effortlessly, users benefit from a seamless journey, sparing them from the frustration of navigating through multiple doors, each with its own rules and requirements. For instance, a patient's electronic health records should be accessible to healthcare providers across different facilities, ensuring continuity of care and a smoother healthcare experience. |
| Accessibility | Improved Access to Information | Interoperability eliminates data silos and enables information to flow freely between systems. This means that individuals can access their data and services more easily and conveniently. For example, in healthcare, patients can securely share their medical records with various healthcare providers, leading to improved care coordination and personalized treatments. |
In this modern digital age, the concept of a "digital front door" has become increasingly relevant, representing the gateway through which individuals and organizations interact with various services, systems, and technologies.
Source: Association of Health Care Journalists, 2022
Unlocking the full potential of the digital front door
Interoperability fosters a connected world that empowers individuals, enhances efficiency, and drives progress through 8 key insights.
-
Enhanced Collaboration and Communication
Interoperability enables different systems and platforms to seamlessly exchange data and communicate with each other. This leads to improved collaboration among stakeholders. Enhanced collaboration ultimately results in better decision-making, improved efficiency, and streamlined processes. -
Cybersecurity and Data Privacy
In an interconnected digital world, interoperability also presents challenges related to cybersecurity and data privacy. Yet, it is also the solution. By establishing common standards and protocols for data exchange, interoperability promotes secure data sharing while ensuring that sensitive information remains protected. This is especially vital in industries like finance and healthcare, where data security is paramount. -
Maximizing Data Utilization
The true value of data lies in its effective utilization. Interoperability ensures that data can flow freely between various applications and systems. This enables data-driven decision-making and the development of innovative solutions. -
Enhanced Patient Care and Safety
By enabling the exchange of accurate and up-to-date patient information, interoperability ensures that healthcare professionals have a complete picture of a patient's medical history, medications, allergies, and test results. This leads to more informed decision-making, reduced medical errors, and enhanced patient outcomes. -
Innovation and Third-Party Services
Interoperability fuels innovation by enabling the development of third-party applications and services that can leverage data from different systems. By providing standardized interfaces and data exchange protocols, interoperability allows developers to create innovative solutions that can seamlessly integrate with existing platforms. This leads to a vibrant ecosystem of applications and services that enhance user experiences and drive continuous technological advancements. -
Seamless User Experiences
Interoperability creates a seamless user experience by eliminating the need for users to switch between different platforms or systems to access information or services. This simplifies interactions, reduces complexity, and enhances user satisfaction. -
Cost Savings and Efficiency Gains
Interoperability leads to cost savings and efficiency gains by reducing redundant processes and improving data accuracy. For example, in healthcare, interoperability reduces the need for manual data entry and duplicate tests, resulting in cost savings for both patients and healthcare providers. -
Scalability and Future-Proofing
Interoperability enables systems to scale and adapt to evolving technological advancements. By adhering to interoperability standards and utilizing standardized protocols, organizations can ensure that their systems can integrate with new technologies and platforms in the future. This future-proofing capability allows for flexibility and scalability, ensuring that organizations can leverage emerging technologies and remain competitive in a rapidly evolving digital landscape.
Health interoperability spending is on the rise
The US digital front door market size was valued at US$565.10 million in 2022 and is expected to expand at a compound annual growth rate (CAGR) of 14.91% from 2023 to 2030 (Grand View Research, 2023).
In a recent survey among CIOs and CMIOs of the top 50 health systems in the United States, 55 percent reported they were planning to spend 5% to 20% more on interoperability in the next year. A further 43% said they anticipated spending at least the same amount.

Source: Health Gorilla, 2023
US Digital Front Door Market
Compound Annual Growth Rate 2023 to 2030: 14.9%
Source: Grand View Research, 2023
Your challenge
Interoperability challenges experienced today by health and healthcare organizations, including providers, researchers, and public health professionals, continue to present difficulties with the usability of health information systems due to their shortcomings in supporting core function capabilities, the provision of essential services, and addressing stakeholder needs.
Examples of Business Capability Challenges Faced by Health and Healthcare Organizations Using HealthIT Today:
| Issues | Examples |
| Data design and capture |
|
| Information integrity and quality |
|
| Inability to use data for analytics and advanced reporting |
|
| Lack of interoperability |
|
Source: Journal of AHIMA, 2017.
This research is designed to help public health and healthcare organizations overcome these challenges by focusing on standards-based interoperability to optimize health outcomes for the individuals and populations they serve at foundational, structural, semantic, and organizational levels.
Challenges reported to be a barrier to health data sharing:
-
50%
Quality of data that is shared -
54%
Lack of technical interoperability -
43%
Lack of data standardization -
29%
Lack of trust between entities -
52%
Timeliness of data that is shared
Source: EHI, 2020
Common obstacles
If creating an interoperable health IT ecosystem is the key to unlocking the future of health and healthcare, and with so many benefits, why is it so difficult to accomplish?
-
Competing interests
- E.g. financial, staff, and other resources, etc.
- Complexity
- Cost
- Lack of coordination between health systems, organizations, and agencies
-
Inconsistent and lack of technical standards
- Numerous software systems with varying data standards
- Divergent health information privacy policies
- Differing approaches to gaining patient/individual consent
- Difficulty getting major EHRs to coordinate with each other
- Data gaps across different EHR applications and networks
- Data silos across the ecosystem that would inform the most urgent and impactful patient and/or population interventions
-
The regulatory landscape continues to become increasingly complex:
- Rule revisions for government-sponsored programs occurring on a yearly basis
- Adds to providers' doubts as to whether technologies like machine learning can adapt to these constant regulatory changes
Overcoming barriers
Share of health and healthcare leaders worldwide who felt the following factors would support them fully utilizing health data:
-
27%
More clarity how data is being used within my hospital/healthcare facility/health agency. -
24%
Availability of data specialists to manage and analyze data. -
23%
Tracking performance metrics/KPIs to measure impact. -
22%
Investing in technology infrastructure within my facility/organization. -
22%
Training/educating staff on usage. -
22%
Investing in cloud-computing tools and services. -
22%
Addressing interoperability/data standards. -
22%
Integrating health/IT informatics as a core operating function.
Source: Philips, 2022
Roadblocks to Interoperability
Two Key Issues
Two key issues – readiness and data sharing challenges – are impeding health and healthcare organizations from achieving interoperability.
Three of the Biggest Challenges
Among stakeholders in the health and healthcare industry, the lack of data standardization, technical interoperability, and data quality were the biggest challenges to health data sharing between data-sharing entities.

Top Five Barriers
The top five barriers to interoperability readiness and implementation among health and healthcare executive management and senior leadership are competing priorities, time for implementation, lack of staff, knowledge of requirements, and lack of funding.
Source: EHI, 2020
Overcoming obstacles
The global adoption of interoperability standards is on FHIR.1
Top Ten Purposes for Interoperability
- Transition of Care
- Receiving Laboratory and Pathology Reports and Results
- Receiving Diagnostic Imaging Reports and Results
- Medication Management
- E-Prescribing of Medications
- Patient Access
- Referral Management
- Public Health Registries and Reporting
- Identifying Patients Accurately
- Clinical Ordering of Diagnostic Tests and Procedures
Survey of 22 member nations of the Global Digital Health Partnership (GDHP, 2020).
FHIR global adoption timeline
-
The Office of the National Coordinator for Health Information Technology
In 2015, the Office of the National Coordinator for Health Information Technology (ONC) adopted FHIR standards as part of its efforts to advance health information exchange and interoperability nationwide. The Trusted Exchange Framework and Common Agreement (TEFCA) – authorized by the US Congress through the 21st Century Cures Act (2019) – aims to create a nationwide Qualified Health Information Network (QHIN) as an output of this interoperability framework. QHINs will simplify connectivity for organizations to securely exchange information to improve patient care, enhance the welfare of populations, generate healthcare value, and enable individuals to gather their healthcare information. Source: HealthLeaders, 2023. -
The Global Digital Health Partnership
On July 20, 2020, The Global Digital Health Partnership (GDHP) – a collaboration of 36 governments and territories, government agencies, and 3 international organizations including the World Health Organization, formed to support the effective implementation of digital health services – published Advancing Interoperability Together Globally. GDHP interoperability activities focus on the adoption and alignment of standards across GDHP members, benchmarking interoperability approaches, and sharing strategies to better enable the exchange of patient data between care providers, organizations, caregivers, and patients. FHIR was found to be key to several interoperability solutions among GDHP member nations. Sources: GDHP, 2020; Health IT Buzz, 2021. -
The US Centers for Medicare and Medicaid Services
In July of 2021, working with the Office of the National Coordinator for Health Information Technology (ONC), the US Centers for Medicare and Medicaid Services (CMS) mandated the use of FHIR for CMS-regulated organizations. Sources: CMS, 2023; Forbes, 2022. -
The World Health Organization
On June 23, 2023, recognizing the importance of interoperability standards in digital health transformation, WHO and standards development organization Health Level Seven International (HL7®) signed a Project Collaboration Agreement to support the adoption of HL7 FHIR interoperability standards, globally. Source: WHO, 2023.
1 FHIR (Fast Healthcare Interoperability Resources) is an application programming interface (API)-focused standard used to represent and exchange health information maintained by the standards development organization HL7 for Healthcare Interoperability. Sources: FHIR, 2022; “FHIR Fact Sheets,” HealthIT.gov, 2023.
Executive Brief Case Study
The future enablement of health interoperability outcomes 2030.
In May 2021, the ONC launched a project called “Health Interoperability Outcomes 2030.” The project asked health and healthcare practitioners (N=700), “What should 2030 look like because of interoperability?” Outcome statements were collected and analyzed for trends, groupings, and combinations. The result was a prioritized set of interoperability outcomes focused on the end state of individuals having internet-based access to their electronic health information, setting the course for aspirational and achievable goals by 2030.
The Office of the National Coordinator for Health Information Technology
INDUSTRY: Government/ HealthIT
SOURCE: The Office of the National Coordinator for Health IT
An aspirational vision of interoperable health systems by 2030.
- The health system will enable evidence-based, precision care that accounts for the social and health conditions of each patient, including links between health and human services.
- The health system will more quickly identify high-risk conditions, chronic diseases, and disparities in health equity.
- The data used for clinical and administrative processes will be electronically integrated to support decisions about payment, eligibility, and benefits.
- Public health response and preparedness will be driven by real-time data that allow public health agencies to quickly identify when and where infectious disease outbreaks occur and maintain insights about health system capacity.
- Reporting for public health, quality measurement, and safety will all be completed automatically and electronically.
- Researchers will be able to use inclusive, representative data sets to compare the real-world performance of treatments, procedures, devices, and drugs.
- Research and testing for new decision support, workflows, and other work processes will be able to be conducted across multiple sites and among different technologies.
- Researchers and health professionals will spend little to no time normalizing data for research and quality activities.
- Preventable data-related safety events will be reduced to zero.
- Health professionals will spend less time on administrative tasks and more time caring for their patients.
- Duplicate diagnostic tests and procedures will be reduced.
Source: “Health Interoperability Outcomes 2030,” HealthIT.gov, 2021. Synthesized statements that reflect respondents’ overall sentiment about what health systems should look like in 2030 because of interoperability.
Info-Tech’s Approach
Unlock the Value of Interoperability
The Info-Tech difference:
- Building awareness and knowledge of interoperability definitions, types, and standards.
- Gauging the impact of interoperability through capabilities mapping assessing defining, supporting, and enabling capabilities for interoperability readiness.
- Learning about interoperability and how it affects both your organization as a whole and IT specifically, including challenges and opportunities.
-
CAPABILITY MAPPING
Use the Capability Mapping Tool as an interoperability readiness assessment process.
Click Here to Access the Capability Mapping Tool -
INTEROPERABILITY ASSESSMENT
Identify interoperability types – foundational, structural, semantic, and organizational – across your organization.
Click Here to Access the Interoperability Primer & Playbook -
Interoperability Implementation With FHIR Integration
Build types and standards into your organization’s interoperability ecosystem one use case at a time.
Click Here to Access The Role of Social Determinants of Health in Value-Based Care Delivery
Additional Info-Tech Resources
The true power behind the digital front door
Follow these best practices to make sure your standards-based implementation requirements are solid.
Interoperability Power Plays
- Build awareness and knowledge of interoperability definitions, types, standards, standards-based implementation, and standards testing and conformance.
- Gauge the impact of interoperability by using the capabilities mapping tool for assessing defining, supporting, and enabling capabilities for interoperability readiness across your organization.
- Develop an information infrastructure that includes all interoperability types, applicable standards, guides, and profiles.
- Choose standards that have been vetted by rigorous testing and conformance efforts.
- Build types and standards into your organization’s interoperability ecosystem one use case at a time (e.g. see Info-Tech’s social determinants of health blueprint).
Blueprint benefits
Developing and deploying world-class interoperating data and analytics exchange to meet today's and tomorrow’s health challenges across health and care ecosystem landscapes including all communities served at the individual, patient, and population levels.
Focusing on five key priorities that are interconnected and equally important to reaching the future interoperable state:
- Building the Right Foundation: Improving data exchange infrastructure, collection, analysis, and sharing across health and healthcare organization information networks.
- Accelerating Data for Action: Tapping into more data sources, promoting health equity, and increasing capacities for scalable outbreak response, nowcasting, forecasting, scenario modeling, and predictive analytics in real-time.
- Developing a State-of-the-Art Workforce: Using next-generation skills for actionable health and care insights.
- Supporting and Extending Partnerships: Breaking down silos, ensuring transparency, addressing policy challenges, and solving problems together.
- Managing Change and Governance: Making sure resources are used wisely, monitoring progress, and supporting strategic innovation for new ways of thinking and working.
Interoperability defined 1.1
What is interoperability ...
Leading industry-wide definitions
-
Healthcare Information and Management Systems Society (HIMSS)
The ability of different information systems, devices, and applications (systems) to access, exchange, integrate, and cooperatively use data in a coordinated manner, within and across organizational, regional, and national boundaries, to provide timely and seamless portability of information and optimize the health of individuals and populations globally. -
Office of the National Coordinator For Health IT (ONC)
The ability of two or more systems to exchange health information and use the information once it is received. -
American Health Information Management Association (AHIMA)
The ability to communicate and exchange data accurately, effectively, securely, and consistently with different information technology systems, software applications, and networks in various settings, and exchange data such that clinical or operational purpose and meaning of the data are preserved and unaltered. -
Institute of Electrical and Electronics Engineers (IEEE)
The ability of two or more systems or components to exchange information and to use the information that has been exchanged.
01 Info-Tech Play
Build awareness and knowledge of interoperability definitions, types, standards, standards-based implementation, and standards testing and conformance efforts.
... and why is it important?
1.0 Info-Tech Insight
Standards-based interoperability in health and healthcare organizations provides timely, safe, and secure access, integration, and use of electronic health data so that it can be used to optimize health outcomes for individuals and populations.
“You can’t manage what you can’t measure.”
– Peter Drucker
“In public health, we can’t do anything without surveillance. That’s where public health begins.”
– David Satcher, MD, PhD, CDC Director 1993–1998, in “DMI Basics,” CDC, 2022
Interoperability defined 1.2
Four types of interoperability

Source: Healthcare IT News, 2019
Interoperability is a journey, not a destination
1.1 Info-Tech Insight
Health and healthcare organizations prioritizing interoperability and standards at all levels will see improvements in data access, integration, management, retrieval of data and documents, scientific staff productivity, IT efficiencies, cost optimization, and data exchange capabilities, ensuring quick, safe, and secure gathering, analyzing, and sharing of electronic health information in ways that follow all industry and HIPAA protocols.
1.2 Info-Tech Insight
Standards-based interoperable HIT solutions are becoming fundamental building blocks driving digital transformation, enabling financial efficiencies, and supporting standards development as well as the implementation, operation, and use of standards-based HIT solutions – specifically for services integration, cloud computing, cybersecurity, and information safety.
02 Info-Tech Play
Gauge the impact of interoperability by using Info-Tech’s capabilities mapping tool for assessing defining, supporting, and enabling capabilities for interoperability readiness across your organization.
Interoperability defined 1.3
Are health information exchange and data sharing the same thing?
“Health Information Exchange”
United States/Canada
“Data Sharing”
European Union
In the United States and Canada, the sharing of health information between entities is referred to as health information exchange. In the European Union, it is often referred to as data sharing.
Overview: Health information exchange, or HIE, provides the capability to electronically move clinical information among disparate health and healthcare organization information systems and maintain the meaning of the information being exchanged.
The Goal: Health information exchange aims to facilitate access to and retrieval of clinical data to provide safe, timely, efficient, effective, and equitable patient-centered care. HIE can also be used by public health authorities to assist in the analysis of the health of populations.
The Term: The Healthcare Information and Management Systems Society (HIMSS) generally defines the term HIE as either a verb or a noun.
Verb: The electronic sharing of health-related data between two or more organizations facilitated by applied standards for use by a variety of stakeholders to inform health and care.
Noun: Organizations within the United States that provide health information exchange technology and services at a state, regional, or national level and often work directly with communities to promote secure sharing of health data.
Source: HIMSS, 2020
Standards development
Making sense of so many standards.
Standards Development
- There are over 40 different types of standards development organizations (SDOs) in the health IT arena. Examples include Health Level Seven (HL7) and Systematized Nomenclature of Medicine (SNOMED).
Accreditation
- An organization may be accredited by the American National Standards Institute (ANSI) or the International Organization for Standardization (ISO).
Types of Standards
-
In order to understand the types of health data standards available for use, these standards are organized into the following specific categories:
- Vocabulary/Terminology
- Content
- Transport
- Privacy and Security
- Identifiers
The Value of Interoperability Standards
2.0 Info-Tech Insight
Standards provide a common vocabulary, code sets, structure, and guidelines that enable interoperability between systems and/or devices.
2.1 Info-Tech Insight
To seamlessly ingest and curate information about an individual or population and improve the overall coordination and delivery of healthcare services, beneficiary services, or population-based interventions, standards permit clinicians, labs, hospitals, pharmacies, payers, patients, health information exchanges, healthcare services organizations, and public health organizations to share data regardless of application or market supplier.
Which standards do I apply for what purpose?
Associating types of standards with types of interoperability.
Foundational
|
Structural
|
Semantic
|
Organizational
|
2.2 Info-Tech Insight
Interoperability standards development works to increase the adoption of emerging and mature health IT standards and facilitates the coordination of work with health and healthcare organizations to further align existing and emerging standards and implementation guidance with strategic healthcare policy goals to achieve improved health outcomes for people everywhere.
2.3 Info-Tech Insight
With the expansion of data and information exchange partners, along with the shift to value-based care, has come a broader range of data types that are available to inform on more complex and integrated health and care decisions, including data pertaining to the social determinants of health, which can include an individual’s housing status, access to reliable transportation and high-quality care, and level of food security.
