- Organizations face pressure to replace and/or consolidate EHRs to meet demands for interoperability, usability, AI readiness, and cost efficiency.
- Mergers and acquisitions have created fragmented EHR environments, hindering unified patient care.
- Healthcare leaders must take a strategic, structured approach to vendor evaluation – prioritizing partners that align with current goals and offer scalable, future-ready capabilities to support evolving clinical, operational, and technological demand.
Our Advice
Critical Insight
- EHR modernization is a system-wide transformation opportunity, not just an IT upgrade. Success depends on defining your future-state capabilities and care experience before exploring solutions and on recognizing that fragmented legacy systems and vendor sprawl pose greater long-term risks than the cost of change. The right EHR unlocks clinical, operational, and financial value, but only if it’s selected to serve strategy, not just software.
Impact and Result
- Identify the latest market trends in EHR systems, including platform consolidation, AI augmentation, and interoperability advancements.
- Determine business needs, critical capabilities, and governance across care settings such as hospitals, long-term care, and behavioral health.
- Analyze system features and leading EHR vendors to guide confident decision-making and reduce technical debt.
- Leverage Info-Tech’s Healthcare EHR Evaluation and Scoring Tool to begin your selection process with clarity and structure.
Modernize Healthcare Systems: A Buyers Guide to Electronic Health Records
Select the right EHR to align clinical priorities, reduce technical debt, and deliver sustainable operational improvements.
Analyst perspective
Lack of governance, alignment, and planning derails EHR consolidation
Healthcare organizations are under mounting pressure to modernize electronic health record (EHR) systems to meet demands for interoperability, AI readiness, and operational efficiency. Fragmented IT environments, especially following M&A activity, introduce workflow silos, technical debt, and hindered care coordination – creating urgency for consolidation or full EHR transitions.
Despite a growing recognition of modern EHR capabilities, many organizations delay transformation due to cost concerns, change management burdens, and the complexity of data migration. Without clear governance and a strategic roadmap, transitions risk disruption and clinician dissatisfaction.
To drive sustainable digital transformation, leaders must align EHR investments with long-term goals – prioritizing solutions that support seamless data sharing, unified workflows, and scalable innovation. This guide helps organizations navigate adoption paths, evaluate vendor capabilities, and make confident, future-ready decisions.
Sharon Auma-Ebanyat
Research Director, Healthcare Industry
Info-Tech Research Group

Modernize Healthcare Systems: A Buyers Guide to Electronic Health Records
Select the right EHR to align clinical priorities, reduce technical debt, and deliver sustainable operational improvements.
EXECUTIVE BRIEF
Executive summary
|
Your Challenge |
Common Obstacles |
Info-Tech’s Approach |
|---|---|---|
|
Organizations face pressure to replace and/or consolidate EHRs to meet demands for interoperability, usability, AI readiness, and cost efficiency. Mergers and acquisitions have created fragmented EHR environments, hindering unified patient care. Healthcare leaders must take a strategic, structured approach to vendor evaluation – prioritizing partners that align with current goals and offer scalable, future-ready capabilities to support evolving clinical, operational, and technological demand. |
Post-M&A EHR integration is often delayed by the absence of an EHR strategic roadmap going into the merger and limited stakeholder alignment. Outdated vendor evaluation criteria miss critical capabilities like AI, analytics, and cloud-native infrastructure. Resource constraints and clinician change fatigue hinder EHR transitions, while traditional evaluations overlook implementation quality and long-term viability. |
Identify the latest market trends in EHR systems including platform consolidation, AI augmentation, and interoperability advancements. Determine business needs, critical capabilities, and governance across care settings such as hospitals, long-term care, and behavioral health. Analyze system features and leading EHR vendors to guide confident decision-making and reduce technical debt. Leverage Info-Tech’s Healthcare EHR Evaluation and Scoring Tool to begin your selection process with clarity and structure. |
Info-Tech Insight
EHR modernization is a system-wide transformation opportunity, not just an IT upgrade. Success depends on defining your future-state capabilities and care experience before exploring solutions, and on recognizing that fragmented legacy systems and vendor sprawl pose greater long-term risks than the cost of change. The right EHR system unlocks clinical, operational, and financial value, but only if it’s selected to serve strategy, not just software.
Healthcare organizations face growing pressure to replace or consolidate EHRs
EHR switching and consolidation are driven by usability and value.
- Usability and Clinician Burnout: Poor usability in legacy EHRs contributes to clinician frustration and burnout, driving organizations to switch to more user-friendly platforms.
- Interoperability and Data Sharing Pressures: New interoperability standards
(e.g. TEFCA, Cures Act compliance) push organizations to consolidate or switch to EHRs with better data sharing and integration. - M&A and Multi-System Complexity: Maintaining multiple legacy systems increases technical debt and operational costs, encouraging consolidation into modern, scalable platforms.
- Cost Containment and Technical Debt Reduction: EHR consolidation post-M&A is not just technically complex but also financially burdensome, deterring timely rationalization.
- AI and Advanced Analytics Readiness: Organizations are adopting modern EHRs to support AI tools, predictive analytics, and advanced reporting capabilities.
Healthcare M&As are driving EHR fragmentation, complexity and technical debt
Recent mergers create fragmented EHRs, increasing interoperability challenges, clinician burden, and technical debt that hinder modernization and raise costs.
- Fragmentation and Complexity Post-M&A: M&As frequently result in the coexistence of different EHRs across newly combined organizations, creating data silos and operational inefficiency.
- Interoperability and Integration Challenges: M&As introduce interoperability barriers when trying to integrate distinct EHR systems or reconcile differing data standards.
- Technical Debt Accumulation: M&A increases technical debt when organizations continue to operate multiple legacy or poorly integrated EHR platforms.
- Vendor Perspectives on Consolidation Costs: EHR consolidation post-M&A is not just technically complex but also financially burdensome, deterring timely rationalization.
Common obstacles of EHR transitions
EHR transitions face challenges from strategy gaps, vendor issues, resource limits, change fatigue, and data migration hurdles.
- Lack of Strategic Roadmap, Governance, and Stakeholder Alignment Post-M&A: Post-merger integrations often falter due to the lack of a unified digital strategy and insufficient stakeholder engagement, resulting in fragmented IT environments and delayed EHR consolidation.
- Outdated Vendor Evaluation Criteria: Traditional evaluation methods may overlook critical capabilities, such as AI integration, advanced analytics, and cloud-native infrastructure, leading to suboptimal vendor selection.
- Resource Constraints and Clinician Change Fatigue: Limited resources and staff burnout can hinder EHR transitions, especially when implementation quality and long-term viability are not adequately considered.
- Inadequate Change Management Practices: Insufficient training and support during EHR implementation can lead to decreased staff morale and resistance to new systems.
- Challenges in Data Migration and Integration: Complexities in migrating and integrating data from legacy systems can result in data loss, inconsistencies, and prolonged transition periods.
Barriers to EHR Modernization
75% of health system executives prioritize digital transformation but face significant resource shortages and budget constraints.
Source: McKinsey, 2024
46% of healthcare facilities still rely on paper fax machines for data exchange, leading to delays in information sharing.
Source: Consensus, 2025
Select the EHR solution fit to drive future organizational transformation
Member Problem: Healthcare leaders face fragmented, outdated EHR environments and lack strategic vendor alignment, limiting their ability to meet evolving interoperability, usability, and AI demands while managing cost and complexity.
Key Insight: EHR modernization is a system-wide transformation opportunity, not just an IT upgrade. Success depends on defining your future-state capabilities and care experience before exploring solutions, and on recognizing that fragmented legacy systems and vendor sprawl pose greater long-term risks than the cost of change. The right EHR unlocks clinical, operational, and financial value but only if it’s selected to serve strategy, not just software.
|
1. Identify Key Market Trends |
1.1 Identify EHR transition challenges 1.2 Analyze the EHR market 1.3 Map priorities 1.4 Identify benefits of modernized EHR systems |
|---|---|
|
2. Define Business Capabilities and Governance Establish clear success criteria and map required capabilities to ensure the next EHR system delivers both clinical and operational value. |
2.1 Analyze the business capability map and organizational goals 2.2 Map priorities and readiness 2.3 Evaluate the current state |
|
3. Assess Solutions Apply defined criteria to evaluate, shortlist, and select vendors offering the best fit for your strategic, technical, and future-ready needs. |
3.1 Identify key features needed for a modern EHR system 3.2 Determine evaluation criteria and score EHR systems 3.3 Shortlist potential vendors 3.4 Avoid common implementation pitfalls |
Navigate key EHR adoption paths
Selecting an EHR transition model demands careful evaluation of clinical workflows, data architecture, and integration complexity to ensure scalability, interoperability, and user adoption.
|
Paper to EHR |
Switching EHRs |
Post-M&A Consolidation |
Same-Vendor Instance Consolidation (e.g. Epic to Epic) |
|---|---|---|---|
|
Description: Organizations moving from paper records to their first EHR system must redesign workflows, digitize historical data, and manage significant cultural change. Benefits:
Challenges:
|
Description: Switching from one EHR vendor to another to meet new strategic, regulatory, or clinical needs. Often done to improve usability, integration, or cost-effectiveness. Benefits:
Challenges:
|
Description: Following mergers or acquisitions, organizations often operate multiple EHRs. Consolidating onto a single platform simplifies data exchange and governance. Benefits:
Challenges:
|
Description: Organizations with multiple instances of the same EHR (like Epic) consolidate onto a single instance to standardize operations across facilities. Benefits:
Challenges:
|
Chart your EHR transition with confidence
Successful EHR transitions demand more than technology – they require strategic alignment, governance, and foresight into the clinical and operational nuances often overlooked.
Paper to EHR | Switching EHRs | Post-M&A Consolidation | Same-Vendor Instance Consolidation (e.g. Epic to Epic) |
|---|---|---|---|
Best Practices:
Often Overlooked: Paper data abstraction planning – what needs to be digitized, scanned, or left archived. Frontline staff input – ignoring this can increase resistance and reduce user adoption. | Best Practices:
Often Overlooked:
| Best Practices:
Often Overlooked:
| Best Practices:
Often Overlooked:
|
Epic EHR consolidation at Beth Israel Lahey Health and Boston Children's Hospital (2023–2025)
A strategic approach to unifying clinical systems across two leading institutions
INDUSTRY: Healthcare
SOURCE: Becker’s Hospital Review, 2023; Healthcare Innovation, 2025; Mass.gov, 2024; HPG, 2025
|
Challenge |
Solution |
Results |
|---|---|---|
|
Beth Israel Lahey Health (BILH) and Boston Children’s Hospital both launched major EHR consolidation efforts using Epic. BILH sought to unify 13 hospitals under one Epic instance, while Boston Children’s moved from a hybrid Cerner-Epic system to a fully integrated Epic platform. Beth Israel Lahey Health:
Boston Children’s Hospital:
|
Beth Israel Lahey Health
Boston Children’s Hospital
|
Beth Israel Lahey Health:
Boston Children's Hospital:
|
AdventHealth’s transition from Cerner to Epic
AdventHealth’s $660M Epic rollout modernized clinical operations, unified workflows, and positioned the health system for scalable digital growth.
INDUSTRY: Healthcare
SOURCE: Seha Consulting, 2025; Becker’s Hospital Review, 2024
Challenge | Solution | Results |
|---|---|---|
AdventHealth, a prominent US healthcare system, operated 37 hospitals using Cerner's EHR platform. Over time, the organization identified limitations in interoperability, scalability, and user satisfaction with the existing system. These challenges prompted the need for a more integrated and efficient EHR solution to support its expansive network and enhance patient care. | In February 2020, AdventHealth announced its decision to transition from Cerner to Epic Systems. The organization embarked on a comprehensive, multiyear implementation plan, partnering with Virtustream to leverage cloud-based infrastructure for the new EHR system. This strategic move aimed to unify patient records, streamline workflows, and improve data accessibility across all facilities. | By February 2024, AdventHealth successfully completed the $660 million Epic rollout across all 37 hospitals. The transition resulted in:
|
The Buyers Guide accelerates your success through the Rapid Application Selection Framework (RASF)
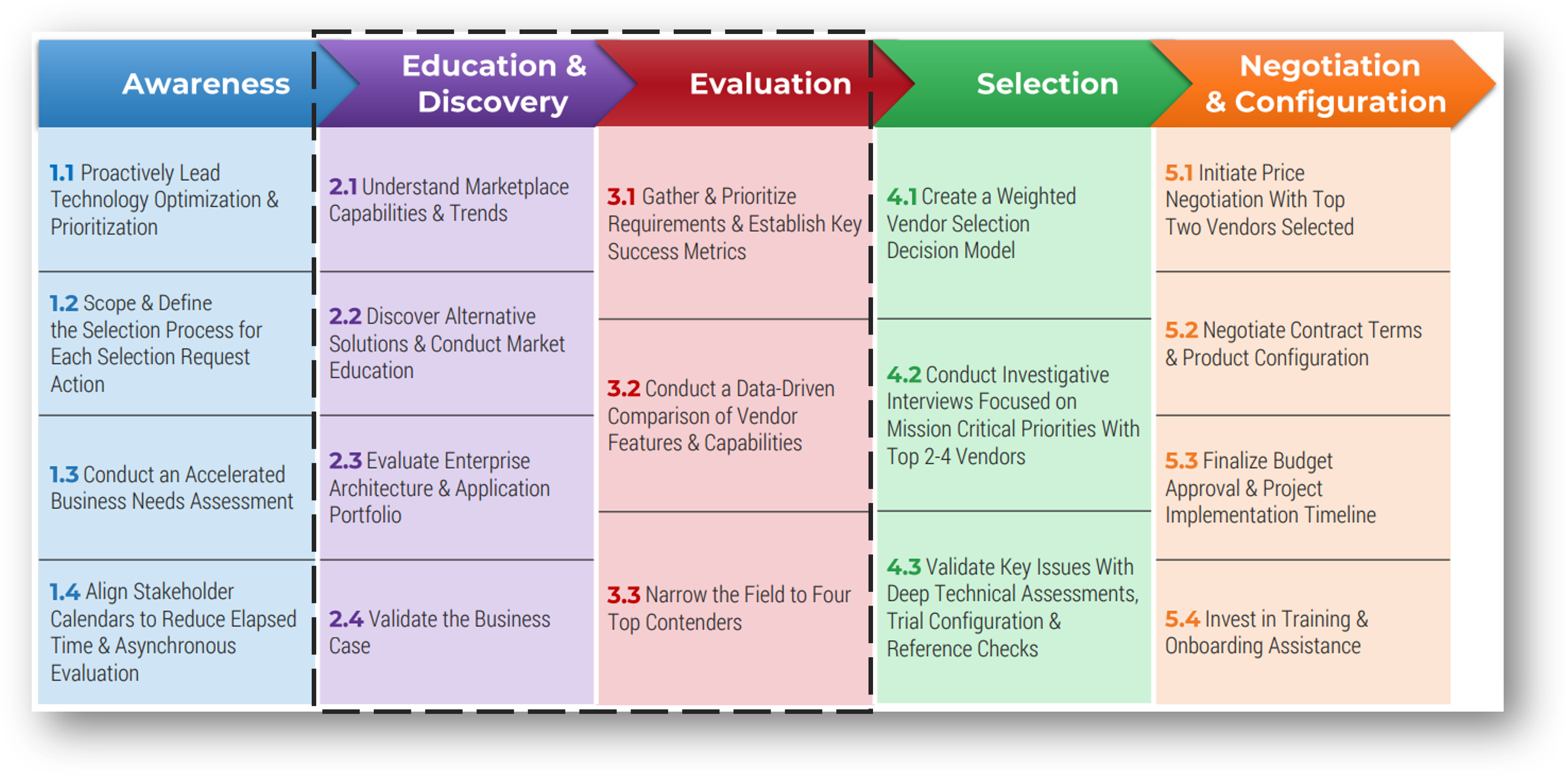
This buyers guide will work through activities within the education & discovery and evaluation phase of RASF. Upon completing this buyers guide, you will be prepared to begin the selection phase, followed by the negotiation & configuration phase, to start your digital transformation.
Download The Rapid Application Selection Framework to learn more
Info-Tech’s methodology selects the EHR solution fit to drive future organizational transformation
1. Identify Key Market Trends | 2. Define Business Capabilities | 3. Identify Assessment Criteria and Assess Solutions | |
|---|---|---|---|
Phase Steps | 1.1 Identify EHR transition challenges 1.2 Analyze the EHR market 1.3 Map priorities 1.4 Identify the benefits of modernized EHR systems | 2.1 Analyze the business capability map and organizational goals 2.2 Map priorities and readiness 2.3 Evaluate the current state | 3.1 Identify key features needed for a modern EHR system 3.2 Determine evaluation criteria and score EHR systems 3.3 Shortlist potential vendors 3.4 Avoid common implementation pitfalls |
Phase Outcomes |
|
|
|
Key deliverable:
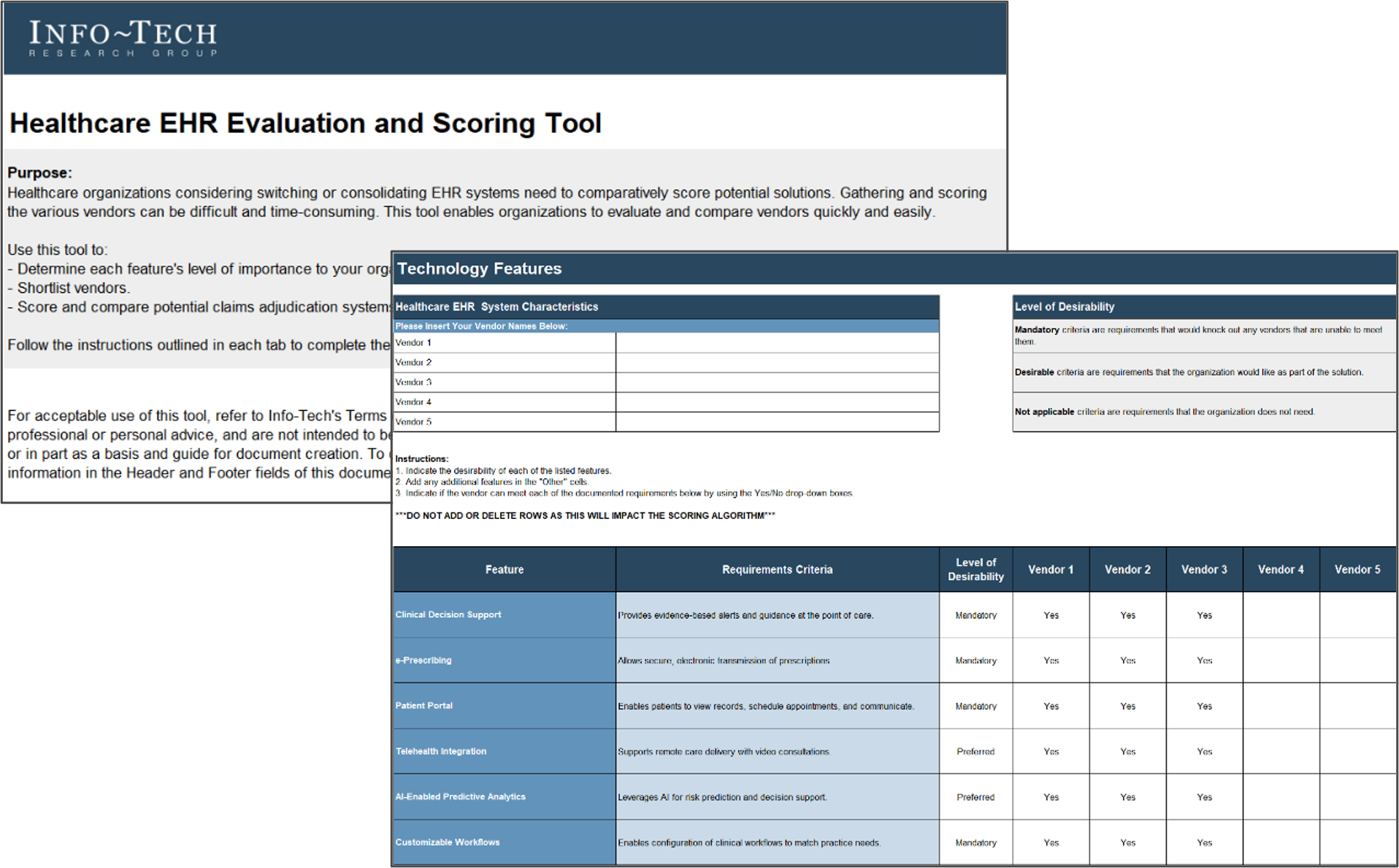
Gathering and scoring the various vendors can be difficult and time-consuming. This tool enables organizations to evaluate and compare vendors quickly and easily.
Use this tool to:
- Determine each feature’s level of importance to your organization.
- Shortlist vendors.
- Score and compare potential EHR systems.
Healthcare EHR Evaluation and Scoring Tool
Guided Implementation
What does a typical GI on this topic look like?
| Phase 1 | Phase 2 | Phase 3 |
|---|---|---|
|
Call #1: Scope objectives of new EHR, and challenges being faced. Call #2: Understand the market and current readiness state. |
Call #3: Identify business goals and align objectives. Call #4: Identify target-state information assessment. Call #5: Identify relationship between current state and expected gains. Call #6: Identify key features that mend the gaps. |
Call #7: Determine evaluation criteria. Call #8: Score and evaluate solutions and Identify next steps. |
A Guided Implementation (GI) is a series of calls with an Info-Tech analyst to help implement our best practices in your organization.
A typical GI is 6 to 8 calls over the course of 4 to 6 months.
Info-Tech offers various levels of support to best suit your needs
| DIY Toolkit | Guided Implementation | Workshop | Executive & Technical Counseling | Consulting |
|---|---|---|---|---|
| "Our team has already made this critical project a priority, and we have the time and capability, but some guidance along the way would be helpful." | "Our team knows that we need to fix a process, but we need assistance to determine where to focus. Some check-ins along the way would help keep us on track." | "We need to hit the ground running and get this project kicked off immediately. Our team has the ability to take this over once we get a framework and strategy in place." | "Our team and processes are maturing; however, to expedite the journey we'll need a seasoned practitioner to coach and validate approaches, deliverables, and opportunities." | "Our team does not have the time or the knowledge to take this project on. We need assistance through the entirety of this project." |
Diagnostics and consistent frameworks are used throughout all five options.
Phase 1
Identify Key Market Trends
| Phase 1 | Phase 2 | Phase 3 |
|---|---|---|
1.1 Identify EHR transition challenges 1.2 Analyze the EHR market 1.3 Map priorities 1.4 Identify the benefits of modernized EHR systems | 2.1 Analyze the business capability map and organizational goals 2.2 Map priorities and readiness 2.3 Evaluate the current state | 3.1 Identify key features needed for a modern EHR system 3.2 Determine evaluation criteria and score EHR systems 3.3 Shortlist potential vendors 3.4 Avoid common implementation pitfalls |
This phase will produce the following deliverables:
- Prioritized list of trends and relevance
This phase involves the following participants:
- CIO
- CMIO/CNIO, finance, procurement, and key clinical stakeholders
- Revenue cycle and patient management leaders
- Compliance and privacy officer
- IT and data architecture lead
EHRs are the backbone of modern healthcare
EHRs have evolved from digital records to integrated platforms uniting care, administration, compliance, and finance.
Core to Care Coordination and Decision-Making
EHRs consolidate patient data into a single platform, improving care coordination and supporting informed, timely clinical decisions across teams.
Enhancing Patient Outcomes
By enabling accurate tracking of patient history, treatments, and medications, EHRs help reduce medical errors and support safer, higher-quality care.
Supporting Clinical Informatics
EHRs act as central data repositories, empowering clinical informatics and advanced analytics to drive better population health management.
Facilitating AI Integration
Modern EHRs integrate AI for predictive analytics, clinical documentation, and diagnostics, enhancing efficiency and supporting clinician decision-making.
Improving Interoperability
EHRs promote seamless data exchange across healthcare systems through Health Information Exchange (HIE) and adherence to data standards.
Overcome challenges with EHR implementations
Successful EHR transitions require clear strategy, stakeholder engagement, robust change management, strong data integrity, and long-term optimization planning.
Develop a Clear Strategic Roadmap
Establish a phased implementation plan with clear objectives, timelines, and measurable outcomes. Engage stakeholders early to secure buy-in and address concerns proactively.
Engage Stakeholders Early and Often
Form multidisciplinary committees, including physicians, nurses, IT staff, and administrative personnel, to participate in vendor selection, workflow design, and testing phases.
Invest in Robust Change Management and Training
Effective training and change management are critical to minimize disruptions and ensure that staff can efficiently use the new EHR system. Implement comprehensive training programs tailored to different user groups. Designate super users to provide ongoing support and address issues promptly.
Plan for Long-Term Optimization and Support
Post-implementation support ensures that the EHR system continues to meet the evolving needs of the organization and its users.
Establish a governance structure to monitor system performance, gather user feedback, and implement necessary updates or enhancements.
Prioritize Data Integrity and Interoperability
Ensuring accurate data migration and system interoperability is essential for maintaining care continuity and avoiding data silos.
Conduct thorough data mapping and cleansing before migration. Choose EHR systems that comply with interoperability standards like FHIR to facilitate seamless data exchange.
